Mental disorders in New Zealand are extremely common, with over a third of adults attending GP practices or nurses (primary care) likely to have met the criteria for a mental illness within the preceding 12 months.
A high proportion of patients in primary care present with medically unexplainable symptoms, that is, a mix of physical and psychological symptoms caused by psychological or life stress.
Maori have a poorer mental health status than non Maori independent of education, income and occupation. Maori have a higher prevalence of mental disorders and tend to access mental health services at a later stage in their illness and tend to present with more severe symptoms.
Pacific peoples fall midway between Maori and non Maori in terms of mental illness prevalence, with a similarly high rate of mental disorders and underutilisation of health services.
Mental disorders are extremely common in NZ with 40% of people experiencing a mental disorder at some point in their lives. Within the 12 months preceding contact with a health service, 5% of people can be classified with a serious mental illness, 9% as moderate, and 7% as mild.
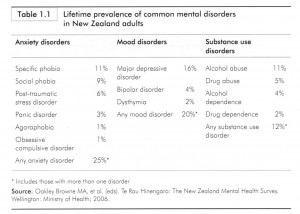
Anxiety disorders are the most common diagnoses in NZ, with a lifetime prevalence of 21%, followed by Depression, Mood Disorders such as Bipolar and Dysthymia (20%) and substance abuse (12%).
Most adults with a psychological disorder have had a diagnosable disorder in childhood. Half of all people with a major mental disorder will have experienced this by age 18, and 3/4 by age 34.
Women have slightly higher overall lifetime prevalence rates of mental disorders (42%) than men (37%).
Women have higher rates of:
- Major Depressive Disorder: 9% higher than men
- Specific Phobia: 7% higher than men
- Post-traumatic Stress Disorder:4% higher than men
- Generalised Anxiety Disorder: 3% higher than men;
Men have higher rates of :
- Alcohol abuse: 9% higher than women,
- Alcohol dependence : 3% higher than women
- Drug abuse: 4% higher than women
- Drug dependence: 1% higher than women;
Of adults attend GP practices, 17% of men and 8% of women will have a substance abuse problem, 12% of men and 22% of women will have depression or dysthymia (a milder longer standing form of depression), and 12% of men and 26% of women will present with anxiety.
However, in one NZ study, only 58 percent of people classified with serious mental health disorders, and 36.5 percent of those with moderate disorders, had visited a health professional about their mental health problem in the preceding 12 months. This left 42 percent of those with a serious disorder who did not receive professional help over that time.
The Ministry of Health believes that there is strong rationale for identification, active management and follow up of mental illnesses in primary care, give ease of access to patients, the potential for early intervention, and the possibility of a holistic and integrated treatment approach. The Ministry recommends extended GP appointments to screen for mental health problems.
References:
- New Zealand Guidelines Group. Identification of Common Mental Disorders and Management of Depression in Primary Care. An Evidence-based Best Practice Guideline. Published by New Zealand Guidelines Group; Wellington: 2008